What is DKD?
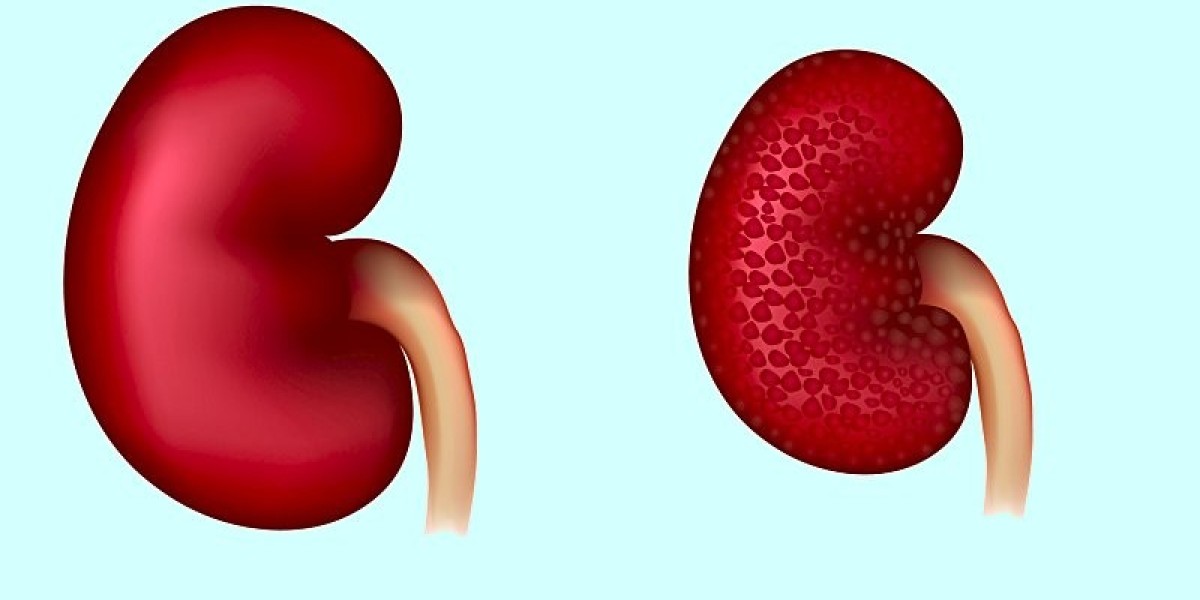
Diabetic kidney disease, also called diabetic nephropathy, is a condition in which the kidneys are damaged due to diabetes. Over time, high blood sugar levels from diabetes can damage the tiny blood vessels in the kidneys, called the glomeruli. This interferes with the kidneys' ability to filter waste from the blood and can lead to serious medical problems.
DKD is a leading cause of end-stage Diabetic Kidney Disease (ESKD). ESKD is when the kidneys have lost most of their function. At this stage, a person often needs regular dialysis or a kidney transplant to survive. Unfortunately, many people with diabetes are unaware they have kidney disease until it has reached an advanced stage. That's why it's so important for people with diabetes to have their kidney function monitored regularly.
Types I and II Diabetes and Kidney Risk
Both type 1 and type 2 diabetes can potentially cause kidney damage over time. However, type 2 diabetes poses a higher risk, as it is far more common. The CDC estimates over 30 million Americans have diabetes, and 90-95% of those cases are type 2.
With type 2 diabetes, high blood sugar levels often go undiagnosed for many years before symptoms appear. This prolonged exposure to elevated glucose increases the risk of diabetic nephropathy. Even after blood sugar levels are brought under control, years of hyperglycemia may have already taken a toll on the kidneys.
In type 1 diabetes, the risk of kidney disease is influenced by factors like blood pressure control and the age at which diabetes was diagnosed. Tight glycemic control from the time of diagnosis improves kidney health outcomes over the long run. But perfect control is difficult, so some degree of diabetic kidney disease remains common with type 1 as well.
Pathophysiology of Diabetic Kidney Damage
At a cellular level, high blood glucose directly damages the tiny blood vessel walls in the kidneys called the glomeruli. Over time, this can lead to thickening and scarring of the glomerular basement membrane.
Some key changes that occur in the pathophysiology of diabetic nephropathy include:
- Glomerular hyperfiltration: Initially, the glomeruli try to compensate for impaired filtration by working harder and filtering more blood. This overworks the kidneys.
- Nephrotic syndrome: Damage to glomerular filtration barriers allows protein to leak into the urine, sometimes causing edema.
- Tubulointerstitial damage: Chronic hyperglycemia also harms the kidney tubules and surrounding tissue, further impairing waste removal.
- Fibrosis and scarring: Over many years, excessive fibrous tissue builds up in the glomeruli and tubules due to persistent cellular damage. This scarring progressively reduces kidney function.
Assessment and Diagnosis of DKD
Because DKD often progresses over many years without noticeable symptoms, timely screening and assessment is crucial. The main ways it is evaluated include:
- Urine albumin tests: Microalbuminuria (moderately high albumin in urine) and macroalbuminuria (very high levels) indicate damage to filtration barriers.
- Estimated glomerular filtration rate (eGFR): This blood test estimates how much blood the kidneys filter each minute. A lower eGFR reflects poorer kidney function.
- Assessment of blood pressure: Hypertension often accompanies diabetic nephropathy and hastens its progression if not controlled.
- Kidney ultrasound: This noninvasive imaging test can detect kidney abnormalities and check size.
The earlier kidney disease is detected, the sooner treatment can begin to help slow its course. Annual screening of urine albumin and eGFR is recommended for all people with diabetes.
Treatment and Management of DKD
While DKD has no cure, a variety of approaches can help control symptoms, delay progression, and preserve quality of life:
- Tight glycemic control: Maintaining near-normal blood sugar levels through medication, diet, exercise reduces further renal damage.
- Strict blood pressure control: Antihypertensive drugs target a systolic pressure below 130 mm Hg to protect the kidneys.
- Lifestyle modifications: Weight loss, smoking cessation, dietary changes like limiting protein can benefit kidney health.
- Medications: ACE inhibitors and ARBs are first-line drugs that block the renin-angiotensin system to protect the kidneys.
- Dialysis: As kidney function declines, dialysis removes waste from the blood if the kidneys can no longer do so effectively.
- Transplant: Once kidneys fail completely, a transplant provides the best outcome, though lifesaving medications are needed to avoid rejection.
In Summary, with diligent management, the risk of progressing to end-stage renal disease can be significantly reduced. Early lifestyle and medical interventions give the best chances of long-term kidney protection.
naufan cmi
322 Blog posts