Researchers in Alberta, Canada, investigated the use of mannitol before and during transportation of patients with intracranial emergencies from peripheral hospitals to tertiary neurosurgical facilities. The focus is on the appropriate use of drugs and the extent to which dose errors may occur. The authors found that the dose error rate was 22%, and slightly more patients received doses that were less than, but not greater than, the recommended dose range of the Brain Trauma Foundation. The findings of this study were reported and discussed in the online publication of the Journal of Neurosurgery, "Mannitol Dose Errors in Intracranial Emergency Agency Transfers," by Cameron A. Elliot, MD, Mark MacKenzie, MD, and Cian O'Kelly, MD.
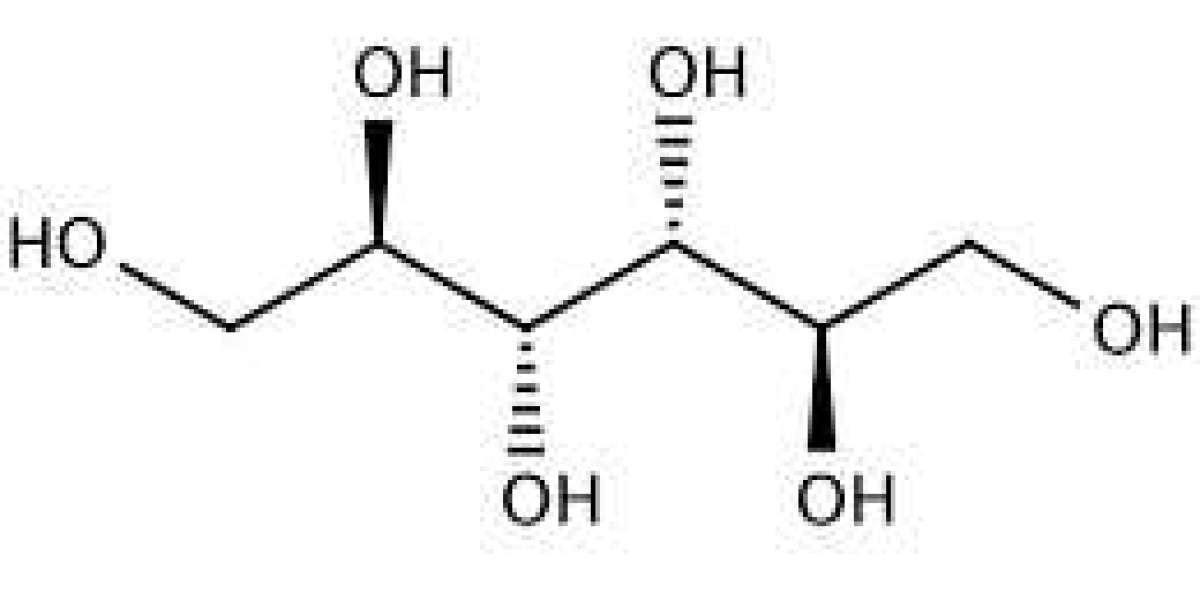
The increase in intracranial pressure may be caused by an increase in cerebrospinal fluid around the brain and spinal cord, an expansion of hematoma, or an increase in pressure within the brain. Elevated intracranial pressure is often accompanied by intracranial emergencies (such as traumatic brain injury or spontaneous intracranial hemorrhage). If the intracranial pressure rises sufficiently high, it may itself constitute an intracranial emergency. If not treated promptly, it may lead to poor prognosis or even death of the patient. Mannitol is commonly used to reduce elevated intracranial pressure. As the author has told us, this drug can be used to bridge the gap between suspected ICP treatment in peripheral hospitals and specialized ICP treatment in tertiary hospitals.
The authors examined data on the amount and duration of mannitol injections for patients with intracranial injury before and during helicopter medical evacuations at tertiary hospitals in Alberta, Canada, from 2004 to 2012. These data are stored in the Shock Trauma Air Rescue Association (STARS) patient database. According to the Brain Trauma Foundation's guidelines for the management of severe traumatic brain injury. This guideline recommends that patients with severe traumatic brain injury (scored 8 or less on the Glasgow Coma Scale), significant progressive neurological deterioration, or unilateral or bilateral pupil fixation and/or enlargement should be given mannitol. The guidelines also recommend that these patients receive mannitol at a dose of 0.25 to 1 gram per kilogram of body weight prior to ICP monitoring. For the purpose of the study, the author believes that less than 0.25 grams per kilogram is insufficient dose, and more than 1.5 grams per kilogram is excessive dose. They define non injection as any infusion that lasts longer than 60 minutes. Because the effect of mannitol is dose dependent, "high doses (1g/kg) provide more durable ICP control." The authors point out that one-time infusion is more effective than continuous administration in reducing ICP.
The STARS database contains information about 120 patients who received mannitol injections during the study period. The authors tell us that according to the study criteria, 86 patients (72%) have appropriate indications for mannitol injection. The use of mannitol was incorrect in 27 patients. Ten patients (8.3%) were under medication and nine patients (7.5%) were over medication. Non pill administration occurred in 8 patients (6.7%).
Due to privacy issues involving data collection and analysis, authors are unable to track individual cases to report patient outcomes. However, they do tell us that given the dose dependent effect of mannitol, a more worrying potential error in mannitol dosage is insufficient dosage, which occurs in 8.3% of cases. The authors point out that the average dose for patients receiving low doses is 0.07 grams per kilogram, which is far below the recommended dose. They also pointed out that a 7% non injection drug delivery rate is of concern because continuous infusion does not affect the rapid decline in ICP compared to high-dose infusion.
Based on their findings, the author plans to work with STARS staff to develop a pre flight checklist of mannitol doses and drug error awareness meetings to reduce the risk of mannitol infusion errors. The authors hope that their findings will improve people's understanding of the frequency of mannitol administration errors. Doctors and other health care providers involved in inter facility transportation can develop other strategies to alleviate this problem. The author plans to involve local transportation stakeholders in this issue and evaluate the effectiveness of their interventions two years after participating and implementing the strategy.