Parkinson's disease (PD) is a progressive neurodegenerative disorder that primarily affects motor function. It is characterized by symptoms such as tremors, stiffness, slowness of movement, and postural instability. These symptoms are largely due to the loss of dopamine-producing neurons in the brain. While medication and physical therapy can manage symptoms, they often become less effective over time. Deep Brain Stimulation (DBS) has emerged as a promising surgical treatment option for Parkinson’s disease, offering hope for improved quality of life.
Understanding Deep Brain Stimulation (DBS)
DBS involves the implantation of electrodes in specific areas of the brain. These electrodes deliver controlled electrical impulses to the brain, which can help modulate abnormal neural activity that contributes to the symptoms of Parkinson’s disease. The electrodes are connected to a small device, known as a neurostimulator or pulse generator, implanted under the skin near the collarbone. This device sends the electrical impulses to the brain through the electrodes.
History and Development of DBS
The concept of using electrical stimulation to treat neurological disorders dates back to the 19th century. However, significant advancements in technology and a deeper understanding of brain function have allowed DBS to become a viable treatment option. The first DBS system was approved by the FDA in 1997 for treating essential tremor, and later, in 2002, for Parkinson's disease. Since then, DBS technology has continued to evolve, with improvements in device design, surgical techniques, and patient outcomes.
How DBS Works
DBS targets specific areas of the brain that are involved in motor control. The most common targets for Parkinson's disease are:
- Subthalamic Nucleus (STN): Stimulation of the STN can help reduce all major motor symptoms of Parkinson’s disease, including tremors, rigidity, and bradykinesia (slowness of movement).
- Globus Pallidus Interna (GPi): Stimulation of the GPi is another effective target for reducing motor symptoms and can be particularly beneficial for reducing dyskinesias (involuntary movements) that can occur as a side effect of long-term medication use.
The choice of target depends on the specific symptoms and needs of the patient. The electrical impulses delivered by the neurostimulator disrupt the abnormal brain activity associated with Parkinson's disease, helping to normalize motor function.
The DBS Procedure
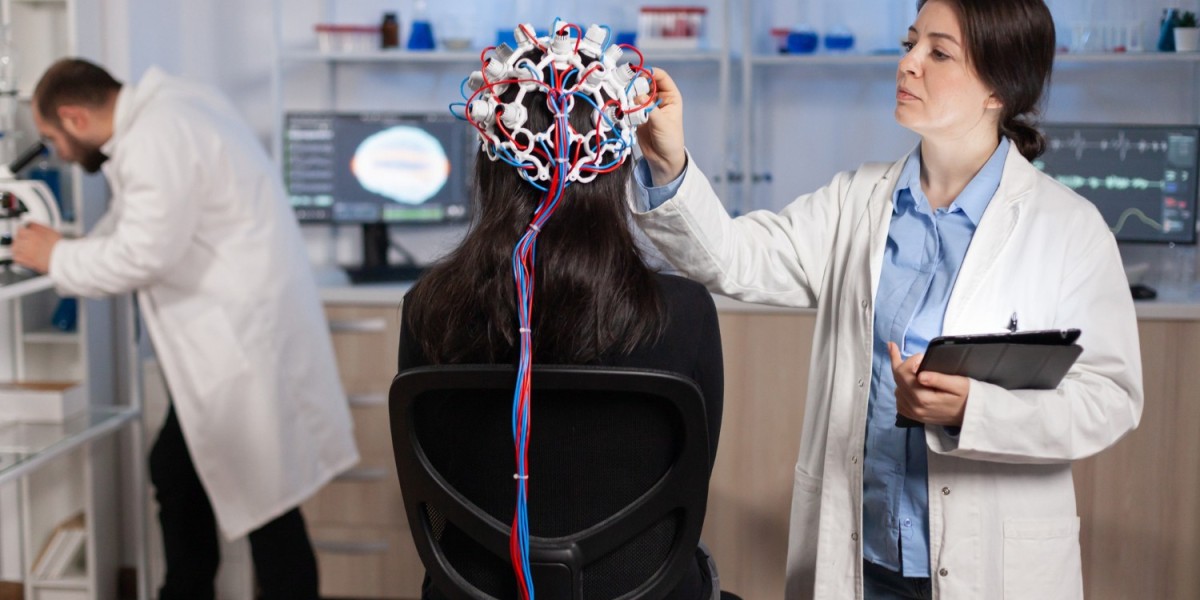
The DBS procedure is typically performed in two stages: implantation of the electrodes and placement of the neurostimulator. Here is a step-by-step overview of the procedure:
- Pre-Surgical Evaluation: Patients undergo a thorough evaluation to determine if they are suitable candidates for DBS. This includes a detailed medical history, neurological examination, imaging studies (such as MRI or CT scans), and neuropsychological testing.
- Surgical Planning: Advanced imaging techniques are used to create a detailed map of the patient’s brain. This helps the surgical team precisely target the areas for electrode implantation.
- Electrode Implantation: The first stage of the surgery involves implanting the electrodes into the targeted brain regions. This is typically done under local anesthesia with the patient awake, allowing the surgical team to monitor brain activity and ensure accurate electrode placement. The patient may be asked to perform certain tasks during the surgery to help guide electrode positioning.
- Neurostimulator Placement: In the second stage, the neurostimulator is implanted under the skin near the collarbone. This is usually done under general anesthesia. The electrodes in the brain are connected to the neurostimulator via extension wires.
- Programming and Adjustment: After surgery, the neurostimulator is programmed to deliver electrical impulses tailored to the patient’s specific needs. This requires multiple visits to adjust the settings for optimal symptom control and minimal side effects.
Benefits of DBS
DBS offers several significant benefits for patients with Parkinson’s disease:
- Improved Motor Function: DBS can significantly reduce tremors, rigidity, bradykinesia, and other motor symptoms, leading to improved overall mobility and quality of life.
- Reduced Medication Dependence: Many patients are able to reduce their medication dosage after DBS, which can help minimize side effects such as dyskinesias and fluctuations in symptom control.
- Long-Term Efficacy: Unlike some other treatments that may lose effectiveness over time, DBS can provide sustained symptom relief for many years.
- Adjustability: The stimulation parameters can be adjusted non-invasively, allowing for personalized treatment and adaptation to changes in symptoms over time.
Risks and Considerations
While DBS is generally considered safe and effective, it is not without risks. Potential risks and side effects include:
- Surgical Risks: As with any surgical procedure, there are risks associated with anesthesia, infection, bleeding, and complications from the implant itself.
- Hardware Complications: There can be issues related to the hardware, such as lead migration, breakage, or battery failure, which may require additional surgeries to correct.
- Side Effects of Stimulation: These can include speech difficulties, balance problems, mood changes, and cognitive effects. However, these side effects can often be managed by adjusting the stimulation settings.
- Non-Motor Symptoms: DBS primarily targets motor symptoms, and while it can improve some non-motor symptoms (such as sleep and mood), it may not address others (such as autonomic dysfunction or cognitive decline).
Patient Selection
Not all patients with Parkinson's disease are suitable candidates for DBS. Ideal candidates typically meet the following criteria:
- Diagnosis: A clear diagnosis of Parkinson's disease with prominent motor symptoms that significantly impact daily life.
- Response to Medication: Good response to levodopa (a common Parkinson’s medication) but with complications such as motor fluctuations or dyskinesias.
- Age and Health: Generally, patients should be under 70 years of age and in good overall health. However, older patients may still be considered on a case-by-case basis.
- Realistic Expectations: Understanding the potential benefits and risks of DBS and having realistic expectations about the outcomes.
- Absence of Contraindications: Conditions such as severe cognitive impairment, psychiatric disorders, or other medical issues that may complicate surgery or postoperative care.
Post-Surgical Care and Follow-Up
Successful DBS treatment requires ongoing care and follow-up. This includes:
- Regular Check-Ups: Frequent visits to adjust the neurostimulator settings and monitor symptom control.
- Medication Management: Adjustments to Parkinson’s medications to complement the effects of DBS and minimize side effects.
- Rehabilitation: Physical therapy and other rehabilitation services to maximize functional improvements and maintain mobility.
- Monitoring and Addressing Side Effects: Continuous monitoring for any side effects and making necessary adjustments to the treatment plan.
- Support and Education: Providing education and support to patients and their families to help them manage the disease and improve their quality of life.
Future Directions and Research
Research into DBS and its applications for Parkinson's disease is ongoing. Some areas of focus include:
- Refining Target Sites: Investigating new brain targets and combinations of targets to optimize symptom control.
- Adaptive DBS: Developing systems that can automatically adjust stimulation parameters based on real-time feedback from the brain.
- Neuroprotective Effects: Exploring the potential of DBS to slow disease progression or provide neuroprotective benefits.
- Combining Therapies: Integrating DBS with other treatments, such as gene therapy or neurotrophic factors, to enhance outcomes.
- Improving Patient Selection: Developing better tools and criteria for identifying the best candidates for DBS.
How Dr. Chirag Solanki Can Help
Dr. Chirag N. Solanki (CNS) is the best neurosurgeon in Ahmedabad in Functional Neurosurgery, including Deep Brain Stimulation (DBS) for Parkinson’s disease. Here’s how Dr. Solanki can assist patients with Parkinson's disease:
Expertise in Functional Neurosurgery
Dr. Solanki is Gujarat’s first Neurosurgeon to specialize in Functional Neurosurgery, bringing advanced surgical techniques and expertise to his patients. His extensive training and experience ensure that patients receive the highest standard of care.
Comprehensive Evaluation
Dr. Solanki conducts thorough evaluations to determine if patients are suitable candidates for DBS. This includes detailed medical history, neurological examination, imaging studies, and neuropsychological testing to ensure the best outcomes.
Personalized Treatment Plans
Understanding that each patient’s needs are unique, Dr. Solanki creates personalized treatment plans tailored to individual symptoms and health conditions. This personalized approach ensures optimal results and improved quality of life.
Advanced Surgical Techniques
Utilizing the latest advancements in surgical techniques and technology, Dr. Solanki performs DBS with precision. His expertise minimizes surgical risks and enhances the success rate of the procedure.
Post-Surgical Care and Follow-Up
Dr. Solanki provides comprehensive post-surgical care, including regular follow-ups to adjust the neurostimulator settings and manage medications. His ongoing support helps patients achieve the best possible outcomes and maintain symptom control.
Multidisciplinary Approach
Dr. Solanki leads Gujarat’s first and only Functional Neurosurgery program with an in-house team of experts. This multidisciplinary approach ensures comprehensive care, addressing both motor and non-motor symptoms of Parkinson’s disease.
Patient Education and Support
Dr. Solanki believes in empowering patients and their families through education and support. He provides detailed information about DBS, its benefits, risks, and post-surgical care, helping patients make informed decisions about their treatment.
Cutting-Edge Research and Innovations
Dr. Solanki stays at the forefront of medical research and innovations in Functional Neurosurgery. By integrating the latest advancements into his practice, he continuously improves treatment outcomes for his patients.
Dr. Chirag Solanki’s dedication to advanced treatment options, protocol-based care, and a humanitarian approach makes him a trusted partner in managing Parkinson’s disease. His expertise in DBS offers hope for patients seeking long-term relief from debilitating symptoms and a better quality of life.
Conclusion
Deep Brain Stimulation has transformed the treatment landscape for Parkinson's disease, offering significant improvements in motor function and quality of life for many patients. While it is not a cure, DBS can provide long-term relief from debilitating symptoms and reduce the reliance on medications. As research and technology continue to advance, the potential benefits of DBS are likely to expand, providing even greater hope for those living with Parkinson's disease.
For patients and caregivers, understanding the intricacies of DBS, including its benefits, risks, and ongoing care requirements, is essential for making informed treatment decisions and achieving the best possible outcomes. Collaborating with a skilled and experienced neurosurgeon, such as Dr. Chirag Solanki, can further enhance the success of DBS treatment. His expertise in Functional Neurosurgery and commitment to personalized, comprehensive care ensures that patients receive the best possible support throughout their treatment journey.
By staying informed and working closely with healthcare professionals, patients with Parkinson's disease can make empowered decisions about their treatment options, leading to improved management of symptoms and a better quality of life.
Read this also:
Minimally Invasive Brain Tumor Surgery Explained
Neurological Disorders: Types, Symptoms, And Treatments
Minimally Invasive Brain Tumor Surgery: Techniques, Benefits, and Recovery